Provider Relations

Meridian is the largest Medicaid health plan in Illinois, and our providers exemplify our mission to deliver the highest quality care to transform the health of communities, one person at a time. Our Provider Relations department is here to assist new and established providers as they fulfill that mission.
Available Support Options
![]()
Secure Provider Portal
The Meridian secure provider portal is available 24/7 and is the fastest way to verify member eligibility, manage claims, authorizations, view patient lists, care gaps, and submit a notification of pregnancy, as examples.
![]()
Provider Relations
Contact your organization's assigned Provider Engagement Administrator or representative for seamless support. For those without an assigned representative, please complete our intake form or contact us using the information below.
Provider Services
Provider Services is available at 866-606-3700 (TTY 711), Monday through Friday, 8 a.m. to 5 p.m.




Statewide Contacts
Long term care: LTCPR@centene.com
Behavioral health: BHPR@centene.com
FQHCs: FQHC@centene.com
Waiver: Waiver_PR_Team@centene.com
General inquiries: ILProviderRelations@mhplan.com
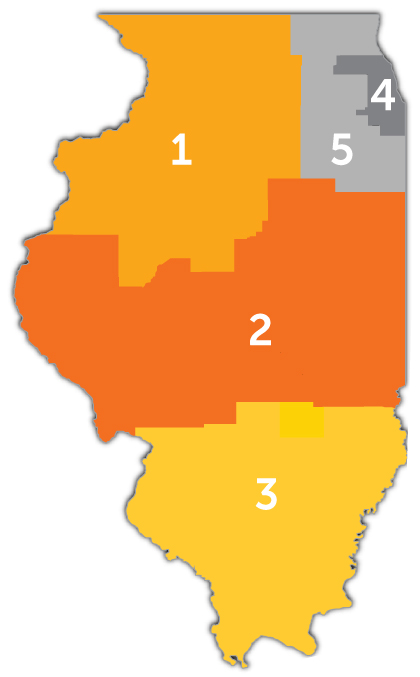
1. Boone
2. Bureau
3. Carroll
4. DeKalb
5. Fulton
6. Henderson
7. Henry
8. Jo Daviess
9. Knox
10. La Salle
11. Lee
12. Marshall
13. Mercer
14. Ogle
15. Peoria
16. Putnum
17. Rock Island
18. Stark
19. Stephenson
20. Tazewell
21. Warren
22. Whiteside
23. Winnebago
24. Woodford
1. Adams
2. Brown
3. Calhoun
4. Cass
5. Champaign
6. Christian
7. Clark
8. Coles
9. Cumberland
10. De Witt
11. Douglas
12. Edgar
13. Ford
14. Greene
15. Hancock
16. Iroquois
17. Jersey
18. Livingston
19. Logan
20. Macon
21. Macoupin
22. Mason
23. McDonough
24. McLean
25. Menard
26. Montgomery
27. Morgan
28. Moultrie
29. Piatt
30. Pike
31. Sangamon
32. Scott
33. Schuyler
34. Shelby
35. Vermillion
1. Alexander
2. Bond
3. Clay
4. Clinton
5. Crawford
6. Edward
7. Effingham
8. Fayette
9. Franklin
10. Gallatin
11. Hamilton
12. Hardin
13. Jackson
14. Jasper
15. Jefferson
16. Johnson
17. Lawrence
18. Madison
19. Marion
20. Massac
21. Monroe
22. Perry
23. Pope
24. Pulaski
25. Randolph
26. Richland
27. Saline
28. St. Clair
29. Union
30. Wabash
31. Washington
32. Wayne
33. White
34. Williamson
1. Cook
2. DuPage
3. Grundy
4. Kane
5. Kankakee
6. Kendall
7. Lake
8. McHenry
9. Will
