Medicaid Billing Requirements Reminder for Home and Community-Based Waiver Services Providers
Date: 11/12/25
The information in this notice applies to Home and Community-Based Services (HCBS) Provider types 90 (Aging), 92 (Persons with Disabilities), 93 (HIV/AIDS) and 98 (Traumatic Brain Injury), who deliver services for the HealthChoice, YouthCare and MMAI (DSNP effective 1/1/2026).
For all claims received on or after 11/20/2025, Meridian will begin validating CMS 1500/837P claims for accurate Medicaid Provider ID numbers. If your claim fails to meet the expectations (see below and in the IAMHP Comprehensive Billing Guide), your claim will be denied with EXWT- WAIVER MUST BILL WITH MEDICAID NUMBER NOT NPI* or EXM1 DENY: NO MEDICAID PROVIDER NUMBER ON FILE**
When billing HCBS services, the provider should only use their Medicaid Provider ID and should NOT send in an NPI on the claim. Further, MCOs require that the Medicaid Provider ID used on the claim matches the provider’s IMPACT registration for the type of waiver service billed. For example, a Medicaid Provider ID registered in IMPACT as an Aging waiver service provider should not be used on a claim for a member who has a TBI waiver.
A valid Medicaid ID must be on the 837P Loop 2010BB in a REF01 Segment qualified by ‘G2’ and the REF02 equal to the provider’s Medicaid ID as registered in IMPACT for their respective waiver provider type.
If the provider has multiple registrations with HFS for provider types outside of the HCBS service realm, the provider should ONLY bill their NPI on the claim for NON-HCBS services.
For example, if the provider is registered as a Home Health provider type (050) and is also registered as a HCBS service provider (090), when billing for Home Health services the provider will bill on an 837I claim format using their NPI in the 2010AA Billing Loop. When billing for HCBS services, the claim must be on an 837P, and use the Medicaid Provider ID, and not an NPI. Refer to the IAMHP Billing manual Home Health section for billing rules to MCOs.
If you are registered with HFS as Provider Type 090, 092, 093 or 098, please be sure to follow the guidance noted in the Home and Community Based Waiver Services section of the IAMHP Comprehensive Billing Guide Section (see section F: Coding Requirements).
837P Submission Guidelines:
Paper Claim CMS-1500 | HIPAA 5010 837P | HIPAA 5010 837P | Waiver Reimbursement |
|---|---|---|---|
Box 24b | 2300 | CLM05-1 | Place of Service Code |
Box 24f | 2400 | SV1-02 | Appropriate procedure code as indicated in the coding grid above |
Box 24j | 2310B | NM1-09 | Should not submit |
Box 31 | DOES NOT MAP IN THE 837 | DOES NOT MAP IN THE 837 |
|
Box 32 | 2310C | NM1 | Service Facility Location Information |
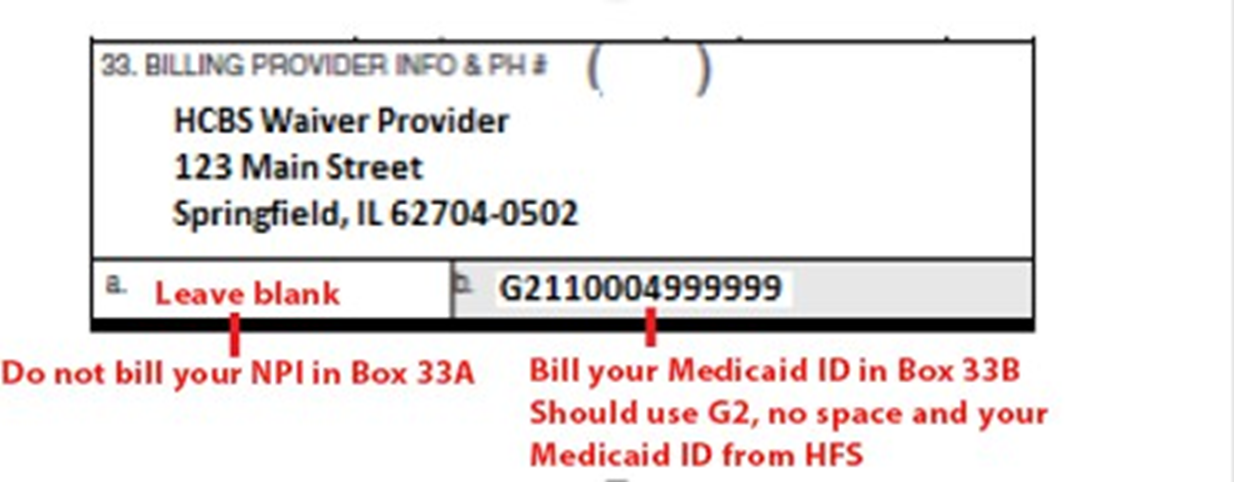
Box 33 | 2010AA | Do not send NPI in NM109 – See 2010BB Loop below | Registered HCBS Organization Name, billing address, HFS Medicaid ID, and applicable taxonomy (as registered in IMPACT). |
Box 33B | 2010BB | REF01 = G2 | HFS Medicaid ID for provider |
Pay to Provider | 2010AB | NM1*87 | Pay to Provider Address (P.O. Box or Lock Boxes acceptable in this loop) ** |
Example of a correctly billed HCBS Waiver claim- no NPI billed, only the Medicaid ID:
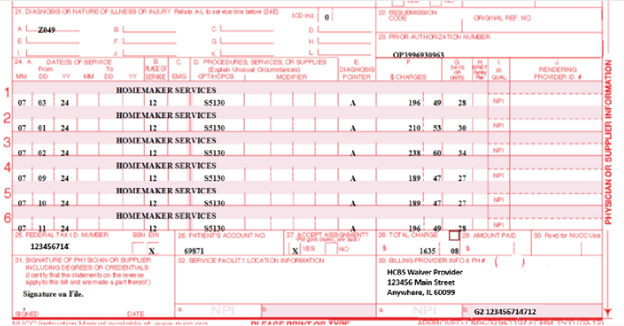
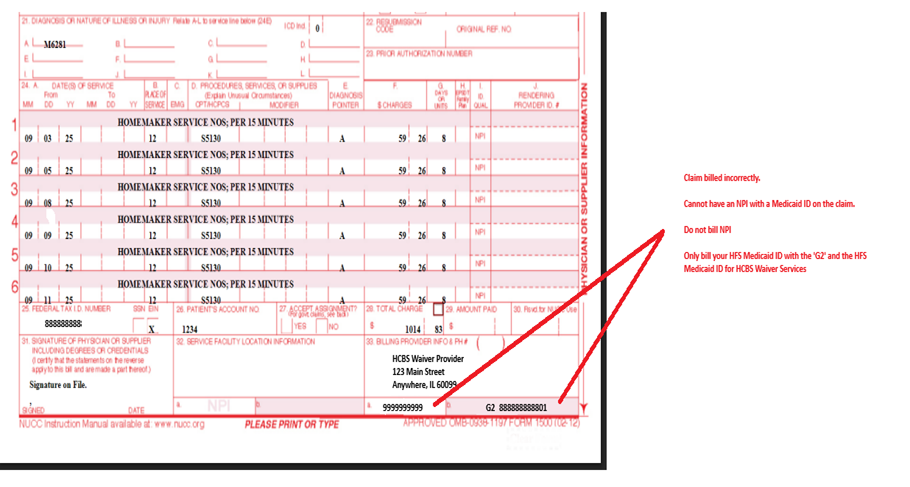
Example of incorrectly billed HCBS Waiver Claim, do not bill an NPI, use your Medicaid ID:
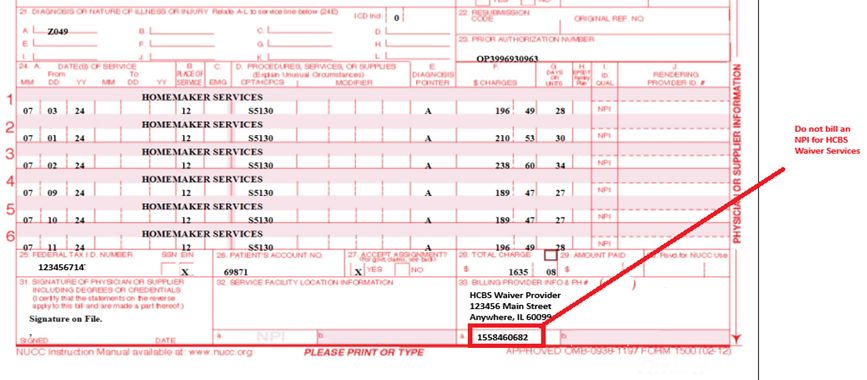
Example of incorrectly billed HCBS Waiver Claim: Only bill the HFS Medicaid ID- Do not bill NPI
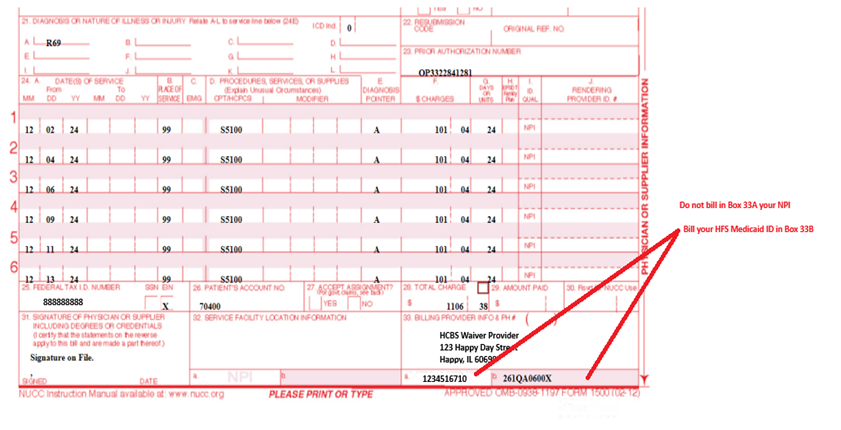
Claim billed incorrectly- Only bill the HFS Medicaid ID- Do not bill the NPI as well
For questions please contact Provider Services at 866-606-3700 or reach out to your Provider Engagement contact. For more information on billing requirements download the IAMHP Billing Guide (PDF).
* CARC A1
** CARC 16/RARC M56