UPDATES TO THE REQUIREMENTS FOR BEHAVIORAL HEALTH CODING BEGIN DECEMBER 1, 2024
Date: 10/15/24
Meridian is committed to offering the highest levels of access, quality, and value in the dynamic healthcare segment of behavioral health. To achieve this goal, and to be in alignment with AMA coding standards, we request your support for correct behavioral health diagnosis reporting.
The goal is to ensure proper diagnosis reporting of:
- Mutually exclusive diagnoses – professional claims only
- Secondary diagnoses reported as primary, first-listed, principle or only.
Effective December 1, 2024, Meridian will expand the coding requirements for behavioral health billing to include the American Medical Association (AMA) coding standards in diagnosis reporting.
In accordance with the Centene Policy for Code Editing Overview (PDF), all providers billing for services using a behavioral health diagnosis are to adhere to the AMA standards. The policy quality and billing integrity requirements will be facilitated by claims editing software, which is updated quarterly to coincide with AMA updates.
Failing to do adhere to AMA published guidelines for billing will result in claim denials. To ensure providers have time to implement compliant billing practices, Meridian would like to highlight the following:
- Mutually exclusive diagnoses – Per the How to Use chapter in ICD 10, “Excludes 1 Note signifies mutually exclusive codes, two conditions that cannot be reported together”. Situations are identified where the excluded diagnosis code in the Excludes 1 Note should never be used at the same time as the code or code range above the Excludes 1 Note. Providers will be allowed to remove the conflicting diagnosis on a corrected claim.
- Secondary diagnosis reported as primary – Situations are identified where a secondary diagnosis code (as identified in ICD10) has been reported as a primary, first-listed, principle or only diagnosis. Providers will be allowed to report additional diagnoses, primary or principle, to the secondary diagnosis on a corrected claim.
Examples of incorrectly coded claims
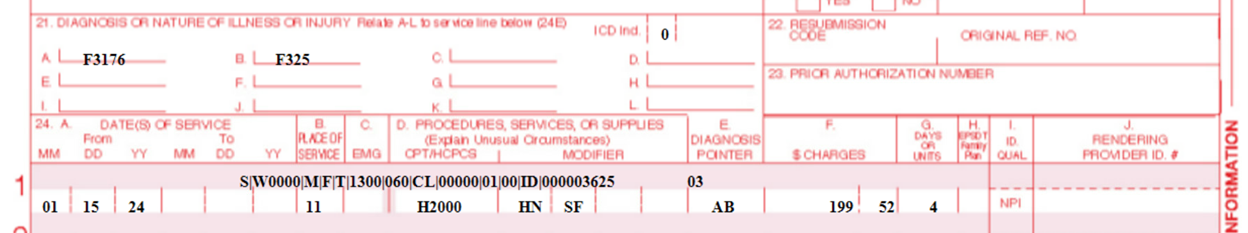
Mutually Excluded Diagnoses
Diagnoses reported F31.76 and F32.5, professional claim with diagnosis pointer to both ICD10 codes. Per code range notes, excludes 1 note on F31— (bipolar disorder) cannot be reported on same line as F32— (major depressive disorder, single episode).
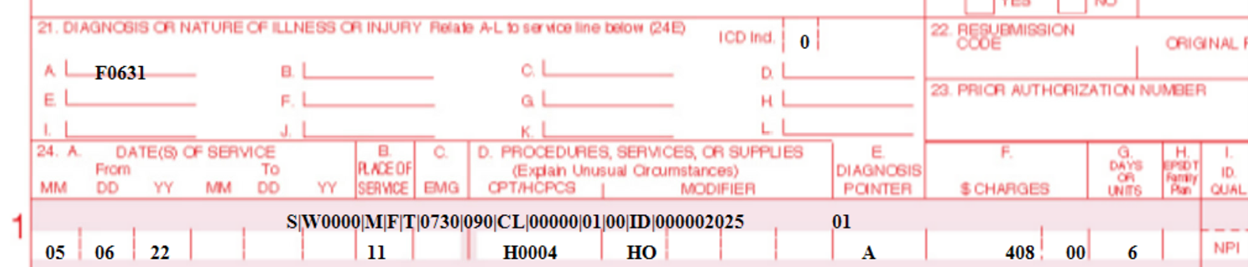
Secondary Diagnosis Reported as Primary:
A diagnosis reported F06.31—professional claim. Per code range notes (F06.-) and code section notes (F01-F09), the underlying condition must be coded first. On this claim, the underlying condition was not reported.
Claims coded incorrectly will deny as EXwd — Diagnosis code incorrectly coded per ICD 10 manual. Providers are encouraged to utilize their diagnosis pointers appropriately (professional claims), code to the highest level of specificity, and cite their own coding resources for more information.
Providers will be allowed to submit corrected claims and will not require medical record review.
- When correcting claims, it is essential that a resubmission code of 6, (corrected) or 7, (replacement) is used to indicate a resubmitted or correct claim.
- If a claim is resubmitted without properly identifying it as corrected, the claim will be denied as a duplicate EX18 or EXDS – duplicate claim.
- Corrected and replacement claims must be submitted within 180 days of the initially denied claim. Failure to do so will result in the corrected or replacement claim being denied for timely filing.
- Providers may also dispute denied claims within 180 days of the payment date. The dispute process is outlined in the Meridian Provider Manual (PDF) available on our Manual, Forms and Resources web page.
Thank you for your support and continued partnership to give Meridian members high quality healthcare. For questions, call Meridian Provider Services at 866-606-3700, Monday through Friday, 8 a.m. to 5 p.m., or contact your Provider Engagement Administrator.
